Healthcare professionals can turn to meditation to improve loneliness and sleep
Study shows Heartfulness Meditation helps improve loneliness and sleep during the Covid-19 pandemic
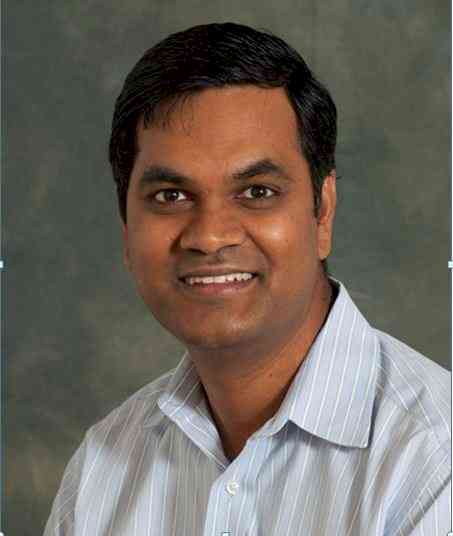
Hyderabad: Unprecedented work pressures and social isolation during the COVID-19 pandemic may worsen loneliness and sleep problems in health-care professionals. But a recent study has shown that Heartfulness Meditation has helped improve loneliness and sleep. The study was conducted by Jayaram Thimmapuram, Robert Pargament, Theodore Bell and Holly Schurk of the WellSpan Hospital, Department of Internal Medicine, York, PA; and Divya K. Madhusudhan of the Harvard Medical School, Department of Graduate Medical Education, Boston, MA.
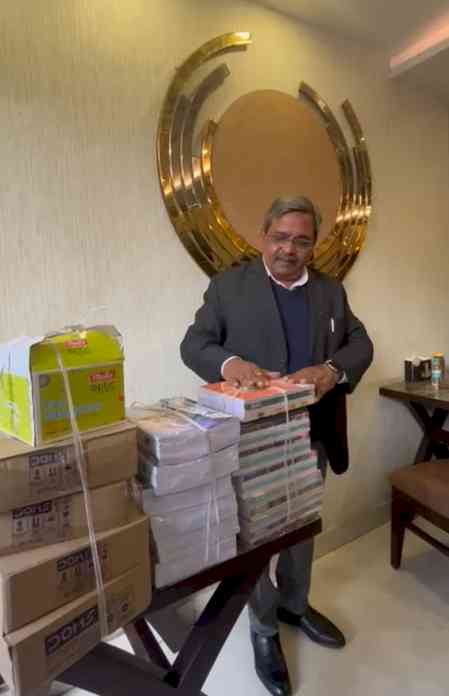
Commenting on the study, Dr. Jayaram Thimmapuram Academic Hospitalist, Internal Medicine, WellSpan York Hospital, York, USA said, “It is one of the first attempts to assess loneliness and sleep problems among physicians and advance practice providers during COVID-19 pandemic in the United States. A significant burden of loneliness and sleep problems were identified. An improvement of sleep and loneliness was noted with the practice of Heartfulness meditation.”
Heartfulness Meditation is a simple heart-based meditation system aimed at attaining a balanced state of mind. A prior study assessing the benefits of Heartfulness meditation practice on resident physicians, nurses and faculty physicians demonstrated improved burnout and emotional wellness along with increased telomere length in a younger subset of population. In patients with chronic insomnia, this practice was associated with favourable outcomes
The objective of this study was to investigate if a brief, virtual, heart-based meditation program via audio relaxation techniques through a Heartfulness trainer leads to measurable changes in improvement of sleep and perception of loneliness in physicians and advance practice providers.
Out of 1,535 eligible participants who were surveyed, 155 enrolled in the study. Sample size was determined by convenience sampling. Participants were randomly assigned to intervention or control groups. Based on a prior study conducted for physicians and advance practice providers within the same organization. All participants were requested to fill out UCLA loneliness and PSQI survey forms prior to randomization. Participants were subjected to computerized randomization. No other intervention was added during the study period.
For any questions related to the study, a Heartfulness trainer was available throughout the study duration. The intervention was virtual with no physical contact with participants during the study period.
All participants in the Heartfulness Meditation group were invited for an orientation session on the aspects of the study and the structure of the meditation protocol. Participants were also briefed about expectations during meditation sessions
Of the 155 enrolled participants, close to a 100 had completed the study, indicating a high attrition rate. The attrition rates in the Heartfulness group were higher compared to the control group. 60–63% in the Heartfulness group completed both pre- and post-intervention surveys as compared to 80–86% of the participants in the control group
The study highlights the significant burden of loneliness and sleep problems among physicians and advance practice providers during COVID-19 with one in two participants feeling lonely and more than nine out of ten having sleep problems. Interestingly, younger participants aged 30 and under had higher loneliness and sleep problems.
Further, as compared to a study conducted in 2018 using a 3-point loneliness questionnaire that showed a prevalence of loneliness in physicians at 43%, the current study reported a higher prevalence among physicians at 47.8%. Although it is difficult to ascribe any of the results to COVID-19 pandemic, increase in loneliness prevalence was notable.
Heartfulness intervention resulted in greater improvements in sleep quality and perception of loneliness when compared with the control group. The findings of this study are consistent with the conclusion of other studies reporting mindfulness-based stress reduction (MBSR) programs and other meditation practices for loneliness and sleep to have demonstrated favourable outcomes.
This study adds to the body of literature supporting the benefits of Heartfulness practice as reported by some of the previous studies utilizing Heartfulness meditation where changes have been noted in heart rate variability, electroencephalography in adults, and improved emotional well-being in school age children.


 cityairnews
cityairnews